Hope for a cure for deadly visceral leishmaniasis
Sist anmeldt: 14.06.2024

Alt iLive-innhold blir gjennomgått med medisin eller faktisk kontrollert for å sikre så mye faktuell nøyaktighet som mulig.
Vi har strenge retningslinjer for innkjøp og kun kobling til anerkjente medieområder, akademiske forskningsinstitusjoner og, når det er mulig, medisinsk peer-evaluerte studier. Merk at tallene i parenteser ([1], [2], etc.) er klikkbare koblinger til disse studiene.
Hvis du føler at noe av innholdet vårt er unøyaktig, utdatert eller ellers tvilsomt, velg det og trykk Ctrl + Enter.
Simone Steger's team's discovery could help develop a treatment for the most serious form of leishmaniasis. Leishmaniasis is a tropical disease affecting an increasing number of people around the world. Between 700,000 and 1 million new cases are reported each year. The causative agent is a protozoan parasite of the genus Leishmania, which is transmitted to humans through the bite of a mosquito. Leishmaniasis includes three clinical forms, of which the visceral form is the most serious.
If left untreated, visceral leishmaniasis is almost always fatal. Most cases occur in Bangladesh, Brazil, Ethiopia, India, Nepal and Sudan.
Professor Steger from the National Institute of Scientific Research (INRS) and her team, in collaboration with other researchers from INRS and McGill University, have observed a surprising immune mechanism associated with chronic visceral leishmaniasis. This discovery could be an important step towards a new therapeutic strategy for this disease. The results of their research were published in the journal Cell Reports.
In many infections, CD4 T cells play a key role in the body's defense. Unfortunately, in the case of chronic infections such as leishmaniasis, maintaining the number of functional CD4 cells becomes important as the immune system is constantly activated to respond to the pathogen.
New immune champions However, research carried out by Professor Steger in her laboratory at the INRS Armand-Frapier Research Center for Biotechnology and Health suggests that these cells may have more than one way of maintaining their viability.
"We have discovered a new population of CD4 cells in mice infected with the parasite responsible for visceral leishmaniasis. These T cells have interesting properties," said Professor Steger.
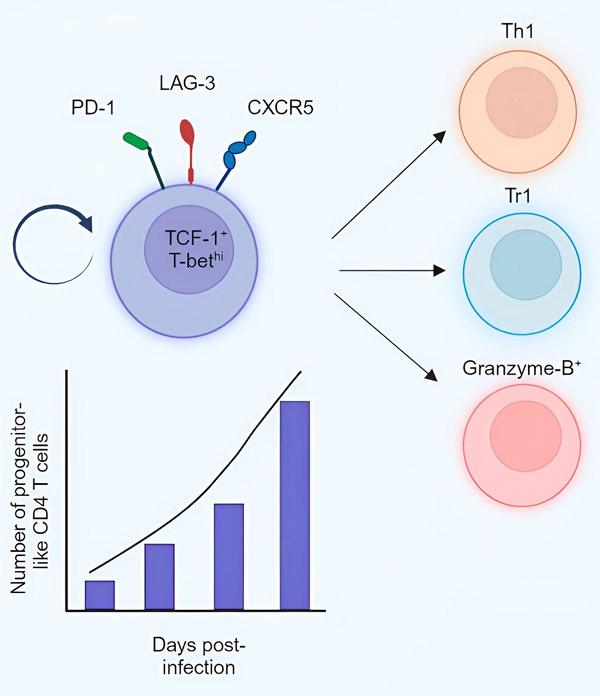
By observing these new cells, scientists noticed that their number increases during the chronic phase of the disease and that, like progenitor cells, they are capable of self-renewal or differentiation into other effector cells responsible for eliminating the parasite, or into regulatory cells that suppress owner's reaction.
Professor Steger notes that CD4 T cells typically differentiate into effector cells from naïve CD4 T cells. But during chronic infections, due to the constant need to generate effector cells, naïve CD4 T cells become severely overloaded and can become exhausted.
"We believe that in the chronic phase of visceral leishmaniasis, the new population we have identified is responsible for the generation of effector and regulatory cells. This will allow the host to prevent depletion of the existing pool of naïve CD4 T cells for a particular antigen," explains the graduate student and first author research, Sharada Swaminiathan.
The new population of lymphocytes discovered by the INRS team may become a crucial immune booster, replacing overloaded naïve CD4 T cells.
“If we can figure out how to direct this new population of lymphocytes to differentiate into protective effector cells, it could help the host get rid of the Leishmania parasite,” Professor Steger said.
Cure for other infections? The study also mentions that similar cells were found in mice infected with lymphocytic choriomeningitis virus and in mice carrying the intestinal worm H. Polygyrus. Thus, it is possible that this population is present in other chronic infections or in other chronic inflammatory environments.
This fact opens up even broader prospects for the discovery made by Professor Steger's team. "If our hypothesis is correct, these cells could be used therapeutically not only for visceral leishmaniasis, but also for other chronic infections," the researcher concludes.
