Nye publikasjoner
Hvorfor har ikke-røykende lungekreftpasienter dårligere resultater?
Sist anmeldt: 02.07.2025

Alt iLive-innhold blir gjennomgått med medisin eller faktisk kontrollert for å sikre så mye faktuell nøyaktighet som mulig.
Vi har strenge retningslinjer for innkjøp og kun kobling til anerkjente medieområder, akademiske forskningsinstitusjoner og, når det er mulig, medisinsk peer-evaluerte studier. Merk at tallene i parenteser ([1], [2], etc.) er klikkbare koblinger til disse studiene.
Hvis du føler at noe av innholdet vårt er unøyaktig, utdatert eller ellers tvilsomt, velg det og trykk Ctrl + Enter.
Forskere fra University College London (UCL), Francis Crick Institute og AstraZeneca har oppdaget årsaken til at målrettede behandlinger for ikke-småcellet lungekreft ikke fungerer hos noen pasienter, spesielt de som aldri har røykt.
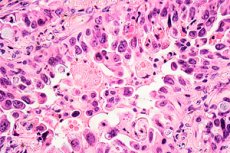
En studie publisert i Nature Communications viser at lungekreftceller med to spesifikke genetiske mutasjoner har større sannsynlighet for å doble sin genomiske belastning, noe som hjelper dem å overleve behandling og utvikle resistens mot den.
I Storbritannia er lungekreft den tredje vanligste krefttypen og den viktigste årsaken til kreftdød. Rundt 85 % av pasienter med lungekreft har ikke-småcellet lungekreft (NSCLC), og det er den vanligste typen hos pasienter som aldri har røykt. Separat sett er lungekreft hos «aldri-røykere» den femte vanligste årsaken til kreftdød på verdensbasis.
Den vanligste genetiske mutasjonen som finnes ved NSCLC involverer epidermal growth factor receptor (EGFR)-genet, som gjør at kreftceller kan vokse raskere. Det finnes i rundt 10–15 % av NSCLC-tilfellene i Storbritannia, spesielt hos pasienter som aldri har røykt.
Overlevelse avhenger av kreftstadiet, og bare omtrent en tredjedel av pasienter med stadium IV NSCLC og en EGFR-mutasjon overlever i tre år.
Lungekreftbehandlinger som retter seg mot denne mutasjonen, kjent som EGFR-hemmere, har eksistert i over 15 år. Mens noen pasienters kreftsvulster krymper med EGFR-hemmere, responderer ikke andre pasienter, spesielt de med en ekstra mutasjon i p53-genet (som spiller en rolle i å undertrykke svulster), på behandlingen og har mye dårligere overlevelsesrater. Men forskere og klinikere har ikke vært i stand til å forklare hvorfor dette er slik.
For å finne svaret, analyserte forskerne data fra studier av AstraZenecas nyeste EGFR-hemmer, osimertinib, på nytt. De så på baseline-skanninger og de første oppfølgingsskanningene tatt etter flere måneders behandling hos pasienter med en EGFR-mutasjon eller en EGFR- og p53-mutasjon.
Teamet sammenlignet hver svulst i skanningene, mange flere enn det som ble målt i den opprinnelige studien. De fant at hos pasienter med kun EGFR-mutasjoner krympet alle svulstene som respons på behandlingen. Men hos pasienter med begge mutasjonene, mens noen svulster krympet, vokste andre, noe som tyder på rask resistens mot legemidlet. Denne typen respons, der noen, men ikke alle områder av kreft krymper som respons på medikamentell behandling hos en enkelt pasient, er kjent som en «blandet respons», og den presenterer en utfordring for onkologer som behandler pasienter med kreft.
For å undersøke hvorfor noen svulster hos disse pasientene var mer utsatt for medikamentresistens, undersøkte teamet deretter en musemodell med både EGFR- og p53-mutasjoner. De fant at innenfor de resistente svulstene hos disse musene hadde mange flere kreftceller doblet sin genomiske belastning, noe som ga dem ekstra kopier av alle kromosomene sine.
Forskerne behandlet deretter lungekreftceller i laboratoriet, noen med bare én EGFR-mutasjon og andre med begge mutasjonene, med en EGFR-hemmer. De fant at etter fem ukers eksponering for legemidlet hadde en betydelig høyere prosentandel av celler med både dobbeltmutasjonen og den doble genombyrden formert seg til nye celler som var resistente mot legemidlet.
Professor Charles Swanton fra University College London og Francis Crick Institute sa: «Vi har vist hvorfor det å ha en p53-mutasjon er assosiert med dårligere overlevelse hos pasienter med ikke-røykende lungekreft, som er en kombinasjon av EGFR- og p53-mutasjoner som gjør at genomet kan dupliseres. Dette øker risikoen for å utvikle medikamentresistente celler gjennom kromosomustabilitet.»
Pasienter med ikke-småcellet lungekreft testes allerede for EGFR- og p53-mutasjoner, men det finnes for øyeblikket ingen standardtest for å oppdage tilstedeværelsen av duplisering av hele genomet. Forskere ser allerede på måter å utvikle en diagnostisk test for klinisk bruk.
Dr. Crispin Highley, fra University College London og onkologkonsulent ved University Hospitals London, sa: «Når vi kan identifisere pasienter med EGFR- og p53-mutasjoner der svulstene viser helgenomduplikasjoner, vil vi kunne behandle disse pasientene mer selektivt. Dette kan bety mer intensiv overvåking, tidligere strålebehandling eller ablasjon for å målrette resistente svulster, eller tidligere bruk av kombinasjoner av EGFR-hemmere som osimertinib med andre legemidler, inkludert cellegift.»
