Nye publikasjoner
Lymfocytter mobiliserer immunforsvaret mot aggressiv brystkreft
Sist anmeldt: 02.07.2025

Alt iLive-innhold blir gjennomgått med medisin eller faktisk kontrollert for å sikre så mye faktuell nøyaktighet som mulig.
Vi har strenge retningslinjer for innkjøp og kun kobling til anerkjente medieområder, akademiske forskningsinstitusjoner og, når det er mulig, medisinsk peer-evaluerte studier. Merk at tallene i parenteser ([1], [2], etc.) er klikkbare koblinger til disse studiene.
Hvis du føler at noe av innholdet vårt er unøyaktig, utdatert eller ellers tvilsomt, velg det og trykk Ctrl + Enter.
Forskere fra det autonome universitetet i Barcelona (UAB) og Instituto della Recherche Hospital del Mar har bekreftet at pasienter med NK-lymfocytter rundt svulstene sine viser bedre respons på behandling. Dette bekrefter muligheten for å bruke cytokiner utskilt av NK-celler som markører for behandlingsrespons ved hjelp av en enkel blodprøve, og støtter bruken av disse lymfocyttene for å forbedre behandlingen hos pasienter med metastatisk HER2-positiv brystkreft.
NK-celler, kjent for sine antitumoregenskaper, er i stand til å aktivere immunforsvaret til å oppdage kreftceller når de kombineres med behandling for den mest aggressive formen for brystkreft. Denne evnen lar dem rekruttere andre immunceller for å bekjempe svulsten.
Oppdagelse av en potensiell biomarkør
Studien, publisert i Journal of Experimental & Clinical Cancer Research, tillot også forskerne å beskrive en potensiell biomarkør for å identifisere pasienter som responderer godt på behandling.
Studien ble ledet av forskere fra Hospital del Mar Institute of Researchs immunitets- og infeksjonsforskningsgruppe, Dr. Aura Muntacell, som også underviser ved UAB, og masterstudent Sara Santana.
Tidligere forskning og nye oppdagelser
Tidligere studier utført av gruppen hadde bekreftet at tilstedeværelsen av NK-celler, en type cytotoksisk lymfocytt som kan drepe tumorceller, i HER2-positive brystkreftsvulster var assosiert med pasienters respons på behandling med anti-HER2-antistoffer. Til tross for denne sammenhengen var antallet deres lavere enn for andre immunsystemceller, noe som førte til at forskerne mistenkte at de også spilte en regulerende rolle i kroppens respons på kreft.
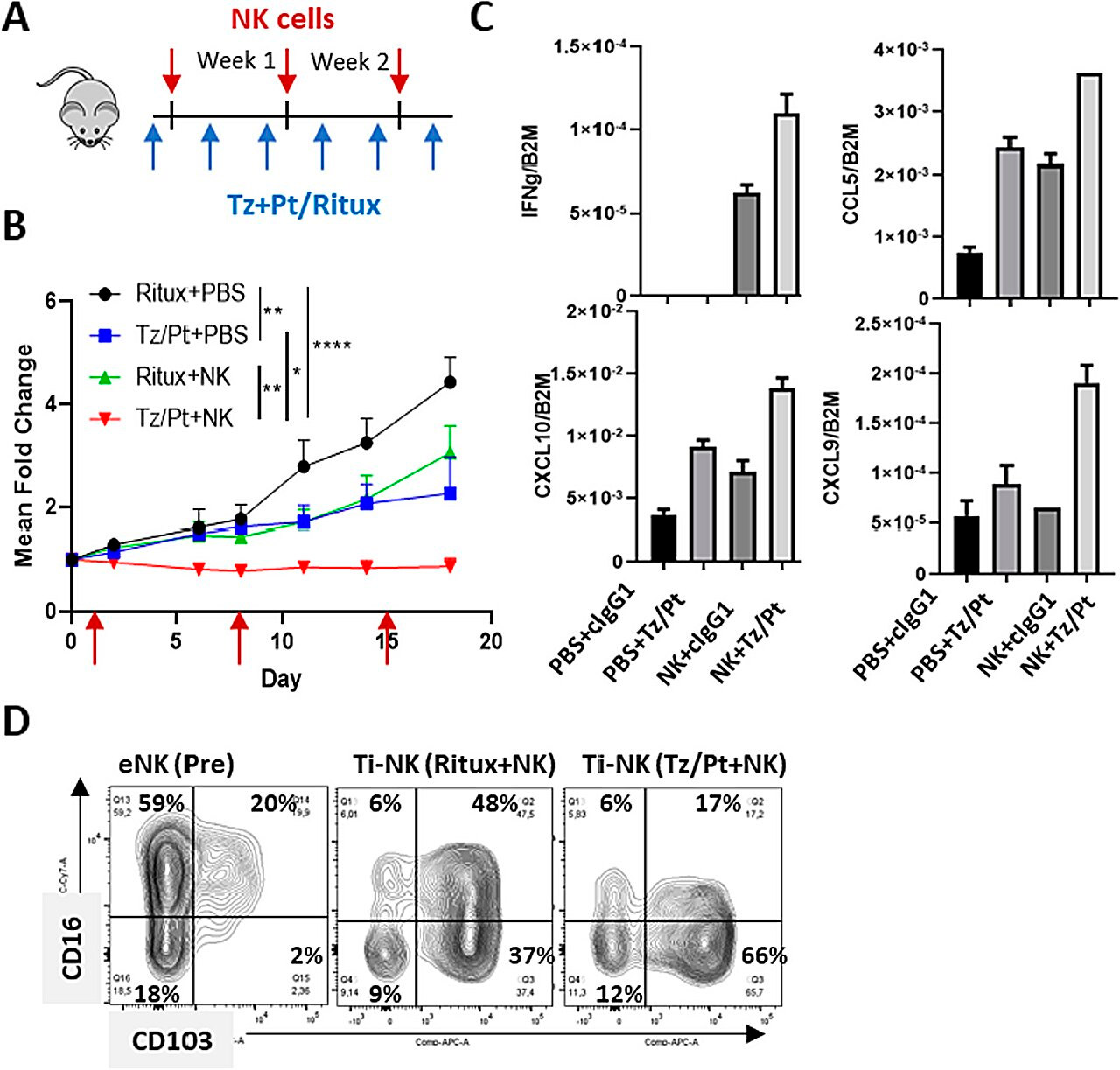
Kombinasjonsbehandling med NK-celler og anti-HER2-antistoffer i en humanisert musemodell av HER2-positiv brystkreft. Kilde: Journal of Experimental & Clinical Cancer Research (2024). DOI: 10.1186/s13046-023-02918-4
En ny studie har fokusert på å belyse dette problemet. Ved å sammenligne RNA-sett fra HER2-positive brystkrefttumorbiopsier med og uten NK-celler, samt musemodeller, kunne arbeidet vise at disse cellene, når de blir utsatt for antistoffer brukt mot disse svulstene, skiller ut to typer små proteiner – cytokiner og andre løselige faktorer.
Dette endrer svulstens mikromiljø, som igjen letter inntredenen av andre immunsystemceller, og forsterker effekten av kreftbehandling.
Potensiell ny biomarkør for behandlingsrespons
Studien så også på om faktorer som frigjøres av NK-celler når de blir utsatt for behandling med anti-HER2-antistoffer, kunne påvises hos pasienter ved bruk av blod- eller serumprøver. Deres tilstedeværelse ble bekreftet gjennom serumprøver fra pasienter under behandling i tilfeller der personen hadde en positiv respons.
«Nye bevis bekrefter evnen til anti-HER2-behandling til å indusere en immunrespons som korrelerer med større terapeutisk effekt. Dette bør tjene som grunnlag for ytterligere forbedring og personalisering av behandlingen for pasienter med HER2-positiv brystkreft», sa dr. Joan Albanell, leder for onkologisk avdeling ved Hospital del Mar, direktør for kreftforskningsprogrammet ved Institute of Research ved Hospital del Mar og en av studiens forfattere.
Oversettelse av funn til andre svulsttyper
Forskerne mener at disse funnene kan være overførbare til andre typer svulster, ettersom studien «beviser at aktiviteten til NK-celler som celler som kan endre svulstmiljøet kan oversettes til andre svulster», forklarte dr. Muntacell.
