Nye publikasjoner
Første kliniske studie viser sikkerhet og effekt av CAR T-terapi mot prostatakreft
Sist anmeldt: 02.07.2025

Alt iLive-innhold blir gjennomgått med medisin eller faktisk kontrollert for å sikre så mye faktuell nøyaktighet som mulig.
Vi har strenge retningslinjer for innkjøp og kun kobling til anerkjente medieområder, akademiske forskningsinstitusjoner og, når det er mulig, medisinsk peer-evaluerte studier. Merk at tallene i parenteser ([1], [2], etc.) er klikkbare koblinger til disse studiene.
Hvis du føler at noe av innholdet vårt er unøyaktig, utdatert eller ellers tvilsomt, velg det og trykk Ctrl + Enter.
Det er for tiden vanskelig å behandle prostatakreft med immunterapi. Resultater fra verdens første kliniske fase 1-studie med kimær antigenreseptor (CAR) T-celleterapi utviklet av forskere ved City of Hope®, en av de største kreftforsknings- og behandlingsorganisasjonene i USA, viser imidlertid at pasienter med prostatakreft trygt kan behandles med cellulær immunterapi med lovende terapeutisk aktivitet, ifølge en fase 1-studie publisert i dag i Nature Medicine.
Studien behandlet 14 pasienter med metastatisk kastrasjonsresistent prostatakreft (mCRPC), som har prostatastamcelleantigen (PSCA) som har spredt seg utover prostata og slutter å respondere på hormonbehandling, med CAR T-celleterapi. Mer enn 34 000 menn med denne typen prostatakreft dør hvert år i USA.
Saul Preisman, PhD, assisterende professor ved City of Hopes avdeling for hematologi og hematopoietisk celletransplantasjon, og kolleger utviklet CAR T-celler som er rettet mot et protein kalt prostatastamcelleantigen (PSCA), som har vist seg å være høyt uttrykt hos pasienter med prostatakreft. Behandlingen involverte å ta pasientens immunceller, kalt T-celler, fra blodet og omprogrammere dem i laboratoriet med CAR for å gjenkjenne og angripe PSCA-proteinet på overflaten av kreftcellene. CAR T-cellene ble deretter infundert tilbake i pasienten for å drepe kreftcellene.
Prostatakreft har blitt kalt en immunørken – tumortåken er vanskelig å behandle med immunterapi fordi det ikke er mange T-celler som kommer inn i svulsten. Det krever noe virkelig kraftig for å overvinne dette. Studien vår viser at City of Hopes CAR T-cellebehandling for prostatakreft kan være et skritt mot å nå dette målet.
Tanya Dorff, MD, PhD, er divisjonsdirektør for City of Hopes program for kjønnssykdommer og professor ved Institutt for medisinsk onkologi og terapeutisk forskning.
«Det viktigste funnet i studien vår er at PSCA-målrettede CAR T-celler er trygge og effektive mot mCRPC», la Priceman til. «Dette åpner muligheten for videreutvikling av denne typen cellulær immunterapi for disse pasientene som for øyeblikket ikke har andre effektive behandlingsalternativer.»
Målene med studien var å undersøke sikkerheten ved behandlingen og dosebegrensende toksisitet, samt å innhente foreløpige data om effekten av behandlingen hos pasienter.
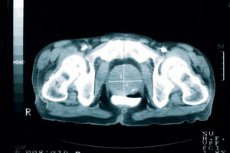
Studiens resultat: Pasientene fikk en enkelt infusjon av 100 millioner CAR T-celler uten forutgående lymfodeplesjonskjemoterapi, som rutinemessig brukes til å behandle blodsykdommer for å øke effektiviteten av CAR T-cellebehandlinger. Fordi dette var den aller første kliniske studien av CAR T-celler, var det viktig å evaluere sikkerheten til CAR T-celler alene hos pasienter. Med samme dose CAR T-celler og lymfodeplesjon oppsto en dosebegrensende toksisitetskomplikasjon av blærekatarr, eller blæreirritasjon. Dorff forklarte at PSCA også er tilstede i blæren, så CAR T-cellene angrep sannsynligvis blæreceller og forårsaket betennelse. Forskerne la deretter til en ny gruppe i studien med redusert lymfodeplesjon, noe som reduserte denne toksisiteten. Fire av de 14 pasientene hadde en reduksjon i PSA-nivåer, en seriemarkør for sykdomsprogresjon hos prostatakreftpasienter, inkludert én pasient med en signifikant reduksjon. Bildene viste behandlingsresponser i en undergruppe av behandlede pasienter. Fem av de 14 pasientene hadde mildt til moderat cytokinfrigjøringssyndrom, som kan være forårsaket av en stor, rask frigjøring av cytokiner i blodet fra immunceller, og er en vanlig bivirkning etter behandling med CAR T-celler. CRS er en behandlingsbar bivirkning. CAR T-cellene vedvarte ikke på høye nivåer utover observasjonsperioden på 28 dager, noe som begrenser behandlingens effektivitet. Dette representerer et vanlig problem innen CAR T-celler for behandling av solide svulster, som forskerne planlegger å ta opp i en oppfølgingsstudie i City of Hope ved bruk av en terapi som nå er tilgjengelig for registrering. Én pasient, som allerede hadde gjennomgått flere tidligere terapier, responderte positivt på CAR T-celleterapi. PSA-nivåene hans falt med 95 %, og kreften i bein og bløtvev krympet også. Han opplevde disse positive responsene i omtrent åtte måneder.
«Pasientens resultater var svært oppmuntrende, og vi er dypt takknemlige for at han deltok i studien vår, samt de andre pasientene og deres familier», sa Dorff. «Vi ønsker å fortsette med denne behandlingen og øke antallet CAR T-celler, og også fortsette å overvåke eventuelle helseproblemer nøye, da vi tror dette kan forbedre behandlingens effektivitet.»
En klinisk fase 1b-studie som bruker PSCA CAR T-celleterapi i kombinasjon med strålebehandling for å forbedre antitumoraktivitet har som mål å inkludere opptil 24 pasienter.
City of Hope, en anerkjent leder innen CAR T-celleterapi, har behandlet nesten 1500 pasienter siden de startet sitt CAR T-terapiprogram på slutten av 1990-tallet. Institusjonen har fortsatt et av de mest omfattende kliniske studieprogrammene for CAR T-celleterapi i verden, med nesten 70 kliniske studier av CAR T-celler på gang, inkludert 13 forskjellige typer solide svulster. Studiene benytter City of Hope-utviklede terapier og produkter fra industrien. En fersk studie publisert i Nature Medicine introduserte City of Hopes CAR T-celleterapi for hjernesvulster.
