Nye publikasjoner
Peptidbasert hydrogel viser lovende resultater for reparasjon av vev og organer
Sist anmeldt: 02.07.2025

Alt iLive-innhold blir gjennomgått med medisin eller faktisk kontrollert for å sikre så mye faktuell nøyaktighet som mulig.
Vi har strenge retningslinjer for innkjøp og kun kobling til anerkjente medieområder, akademiske forskningsinstitusjoner og, når det er mulig, medisinsk peer-evaluerte studier. Merk at tallene i parenteser ([1], [2], etc.) er klikkbare koblinger til disse studiene.
Hvis du føler at noe av innholdet vårt er unøyaktig, utdatert eller ellers tvilsomt, velg det og trykk Ctrl + Enter.

Ved å kombinere biomedisinsk presisjon og naturinspirert ingeniørfag har et team av forskere ledet av University of Ottawa laget et gelélignende materiale som viser et enormt potensial for raskt å reparere et bredt spekter av skadede organer og vev i menneskekroppen.
Banebrytende forskning ledet av førsteamanuensis Dr. Emilio I. Alarcon ved University of Ottawa, medisinske fakultet, kan påvirke livene til millioner av mennesker i fremtiden med peptidhydrogeler som kan forsegle hudsår, levere terapeutiske midler til skadet hjertemuskel og reparere skadede hornhinner.
«Vi bruker peptider til å lage terapeutiske løsninger. Teamet henter inspirasjon fra naturen for å utvikle enkle løsninger for sårlukking og vevsreparasjon», sier Dr. Alarcon, en forsker og direktør for BioEngineering and Therapeutic Solutions (BEaTS)-gruppen ved University of Ottawa Heart Institute, hvis banebrytende forskning fokuserer på å utvikle nye materialer med vevsregenereringsevner.
Peptider er molekyler som finnes i levende organismer, og hydrogeler er et vannbasert materiale med en gelignende tekstur som har vist seg nyttig for terapeutiske formål.
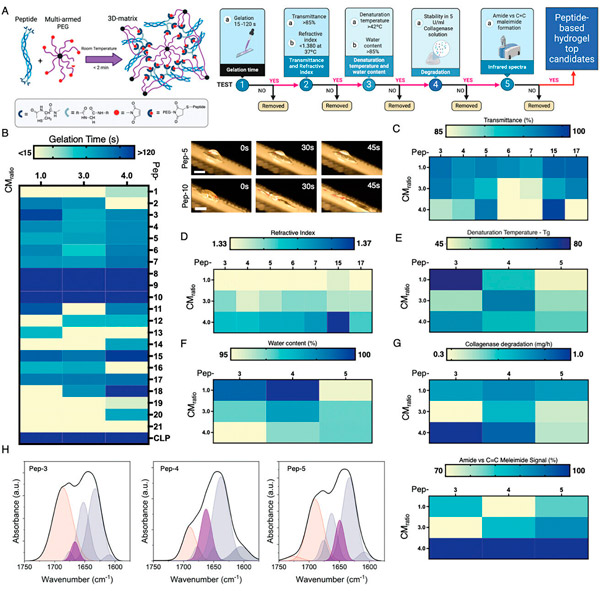
Tilnærmingen som ble brukt i studien, publisert i Advanced Functional Materials og ledet i fellesskap av Dr. Erik Suuronen og Dr. Mark Ruel, er unik. De fleste hydrogeler som studeres i vevsteknikk er animalsk avledede og proteinbaserte, men biomaterialet som lages av det felles teamet er forbedret med konstruerte peptider. Dette gjør det mer anvendelig i klinisk praksis.
Dr. Ruel, professor ved Institutt for cellulær og molekylær medisin ved Universitetet i Ottawas medisinske fakultet og forskningsleder ved avdelingen for hjertekirurgi ved University of Ottawa Heart Institute, mener funnene i studien kan være revolusjonerende.
«Til tross for årtusener med evolusjon, er den menneskelige responsen på sårheling fortsatt ufullkommen», sier dr. Ruel. «Vi ser unormal arrdannelse fra hudsnitt til øyeskader og hjertereparasjon etter et hjerteinfarkt. Dr. Alarcón, Dr. Suuronen og resten av teamet vårt har fokusert på dette problemet i nesten to tiår. Dr. Alarcóns artikkel i Advanced Functional Materials representerer en ny måte å gjøre sårheling, organheling og til og med grunnleggende arrdannelse etter kirurgi mye mer terapeutisk håndterbar og derfor optimalisert for menneskers helse.»
Syntetiserte peptider for umiddelbar reparasjon av bløtvev. Avanserte funksjonelle materialer (2024). DOI: 10.1002/adfm.202402564
Nøkkelen er faktisk evnen til å modulere peptidbiomaterialet. Hydrogelene til teamet fra University of Ottawa er designet for å være tilpassbare, noe som gjør det tøffe materialet tilpasningsdyktig for bruk i et bredt spekter av vev. I hovedsak kan tokomponentoppskriften justeres for å øke klebeevnen eller redusere andre komponenter, avhengig av kroppsdelen som trenger reparasjon.
«Vi ble veldig overrasket over omfanget av bruksområdene materialene våre kan oppnå», sier Dr. Alarcon. «Teknologien vår tilbyr en integrert løsning som er tilpasset målvevet.»
Dr. Alarcon bemerker også at disse studiene tyder på at de terapeutiske effektene av biomimetiske hydrogeler er svært effektive, og at bruken av dem er betydelig enklere og mer kostnadseffektiv enn andre metoder for regenerering.
Materialene ble utviklet til lave kostnader og i et skalerbart format, noe som er en kritisk egenskap for mange storskala biomedisinske applikasjoner. Teamet utviklet også et raskt screeningssystem som reduserte utviklingskostnader og testtider betydelig.
«Denne betydelige reduksjonen i kostnader og tid gjør ikke bare materialet vårt mer økonomisk levedyktig, men akselererer også potensialet for klinisk bruk», sier dr. Alarcon.
Hva er de neste stegene for forskerteamet? De vil gjennomføre store dyreforsøk som forberedelse til testing på mennesker. Så langt har hjerte- og hudforsøk blitt utført på gnagere, og hornhinnearbeidet har blitt gjort ex vivo.
